Taking control of your hormonal health starts with understanding your baseline testosterone levels. In the UK, a man's testosterone typically peaks in his late teens or early twenties. From around age 30, it begins a slow, natural decline, with levels dropping by about 1-2% each year. This guide provides the actionable steps you can take to manage this process.
Your Guide to UK Testosterone Levels by Decade
Testosterone is a cornerstone hormone, influencing everything from muscle and energy to mood and sex drive. But what counts as a “normal” level isn't a fixed number; it's a moving target that changes as you age.
Think of it like physical strength—what’s typical for a 25-year-old is a world away from what’s expected at 55. This gradual decline is a standard part of ageing. For most men, the change is so slow it's barely noticeable year on year. But over a decade, the cumulative effect can become much more obvious.
Understanding these shifts is the first step. It helps you establish a personal baseline and spot when something might be off for your age group, empowering you to take action.
What Is a Normal Testosterone Level?
In the UK, testosterone is measured in nanomoles per litre, or nmol/L. While different labs may use slightly different ranges, a healthy young man will typically have a total testosterone level between 12 nmol/L and 35 nmol/L. As you get older, this range naturally drifts downwards.
A recent UK study of nearly 1,500 men highlighted this trend. It found that men aged 20–24 had an average range of 14.2 to 19.3 nmol/L. Compare that to men aged 40–44, whose range was lower at 12.1 to 16.4 nmol/L. To dig into the numbers, Medichecks offers a great breakdown of these age-related findings.
Use this table to get a clearer picture of the typical ranges you can expect across the decades.
Typical UK Testosterone Levels by Age Group (nmol/L)
This table provides a quick reference for the expected range of total testosterone levels for men across different decades.
| Age Group | Typical Range (nmol/L) | Key Considerations |
|---|---|---|
| 20-29 | 12 - 35 | Peak levels. This is your body's prime for muscle building and vitality. |
| 30-39 | 10 - 30 | The slow, gradual decline begins, typically dropping by 1-2% per year. |
| 40-49 | 9 - 28 | The effects of the decline might start becoming more noticeable now. |
| 50-59 | 8 - 25 | Symptoms of lower T are more common, but levels are still within a wide range. |
| 60+ | 7 - 23 | Levels continue to decline, and monitoring for low T symptoms becomes more important. |
Remember, these are general guidelines. Your personal 'normal' can be influenced by genetics, lifestyle, and overall health.
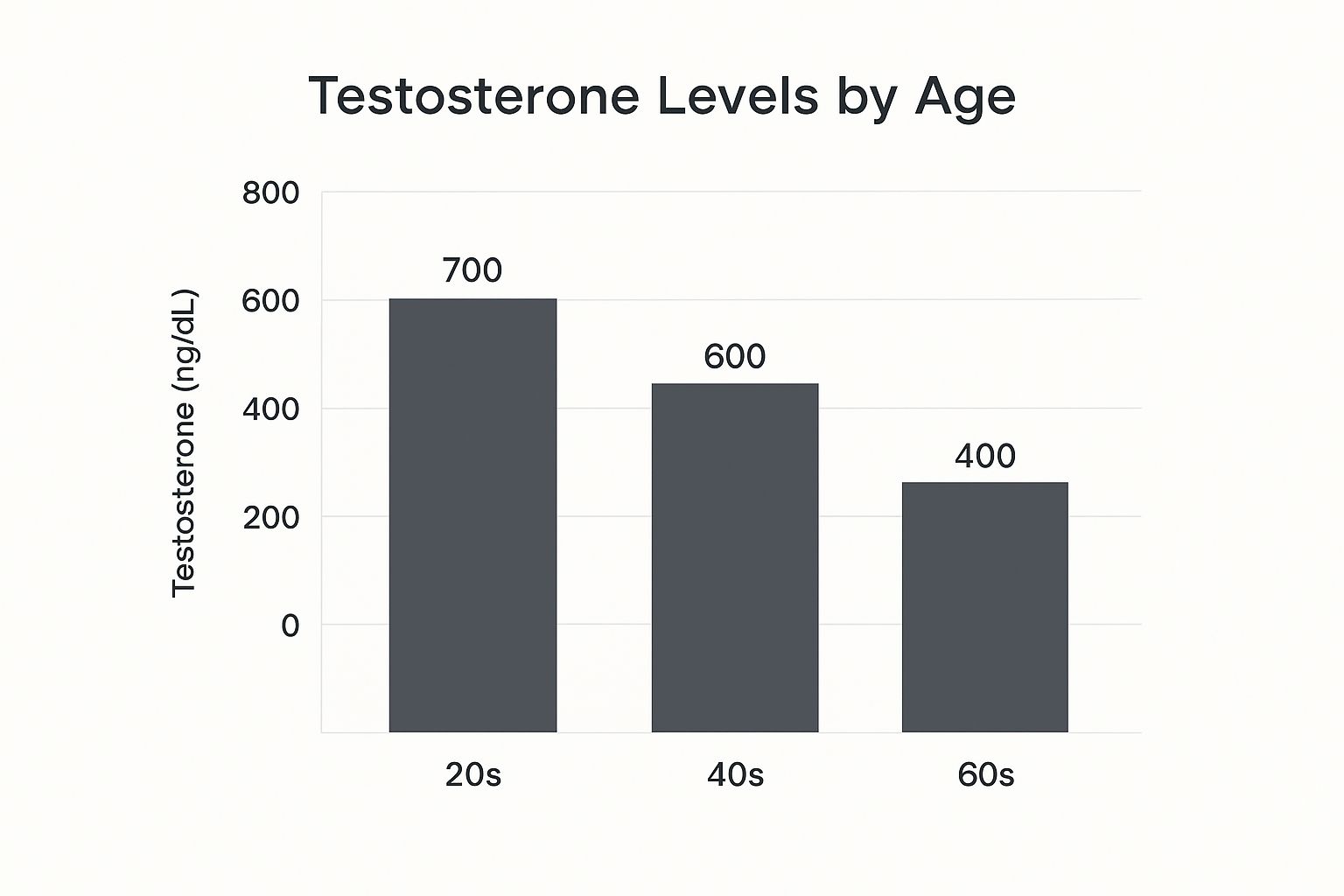
As the chart shows, there's a clear and steady downward trend as you move from your 20s right through to your 60s.
The key takeaway is this: a lower testosterone reading in your 50s might be perfectly normal for your age, but that same reading in your 20s could signal something that's worth a chat with your doctor.
Ultimately, your focus shouldn't just be on the number, but on how you feel. Symptoms often paint a much clearer picture than a blood test alone. Use this guide to understand both the numbers and the real-world signs tied to your changing testosterone levels by age.
Why Your Testosterone Naturally Changes Over Time

Knowing what your testosterone levels are is one thing. But the real power comes from understanding why they change as you get older.
Think of your body's hormone production like a sophisticated factory. In your youth, it runs at peak capacity. But over the decades, it naturally streamlines its operations, leading to a slow and steady reduction in output.
This isn't a glitch in the system; it’s biology. After peaking in your late twenties, the signals from your brain telling the testes to produce testosterone become a little less frequent and powerful. It’s a very subtle shift that happens year after year.
But it’s not just about producing less. The way your body uses testosterone also changes, which brings another key player into the story.
The Role of SHBG: The Hormone Gatekeeper
As we age, our bodies produce more of a protein called Sex Hormone-Binding Globulin (SHBG). Its job is to bind to testosterone in your bloodstream.
Think of SHBG as a security guard that locks onto testosterone molecules, effectively taking them out of circulation.
Once testosterone is bound to SHBG, it’s no longer "free" or "bioavailable." This means your cells can't use it for vital jobs like building muscle or maintaining energy. So, even if your total testosterone only dips slightly, a rise in SHBG can dramatically reduce how much usable testosterone you actually have.
This is a crucial point: you might have plenty of testosterone, but if most of it is locked up by SHBG, you won’t feel the benefits. It’s the difference between having money in a high-security vault versus cash in your wallet.
This gradual increase in SHBG is one of the main reasons why the effects of declining testosterone levels by age become more noticeable over time.
Your Daily Rhythm Flattens Out
Another piece of the puzzle is the change in your body’s daily hormonal clock. For younger men, testosterone production follows a clear daily pattern—it’s highest first thing in the morning and then slowly drops throughout the day.
As you get older, however, this peak-and-trough rhythm starts to flatten out.
Data from the UK shows that while men under 40 can see their levels fluctuate by up to 30-35% in a single day, this variation shrinks to about 10% by the time they reach 70. This shift leads to a more consistent, but lower, overall testosterone presence. You can learn more about the science behind these normal testosterone level changes.
Understanding these natural mechanics is the first step toward taking control. When you know the "why" behind these shifts, you can make smarter lifestyle choices to support your hormonal health as you age.
Recognising the Signs of Low Testosterone
Understanding the numbers is a great start, but those figures only tell half the story. The other, more personal half is all about how you actually feel day-to-day. A drop in testosterone isn't always a sudden crash; it’s often a slow burn of subtle changes you might initially shrug off as just stress or getting older.
Recognising these symptoms is the first actionable step towards figuring out if your levels are lower than they should be. It’s about connecting the dots between how you feel physically, mentally, and emotionally.
This isn't about self-diagnosis, but about building awareness. Knowing what to look for empowers you to have a much more informed conversation with a doctor if you feel something isn’t quite right.
From Lab Results to Lived Experience
The symptoms of low T rarely appear all at once. They tend to creep in as your levels dip below certain thresholds, painting a clearer picture of how numbers on a page translate into real-world feelings.
A slight dip, for example, might first appear as nagging tiredness. As levels fall further, you could notice more significant changes in mood or physical performance. This gradual response is key to understanding why some symptoms show up before others.
Research has even put numbers to these feelings. For instance, low energy can become noticeable around 15 nmol/L, stubborn weight gain at 12 nmol/L, and a persistently low mood at 10 nmol/L. More serious issues like erectile dysfunction tend to become more common when levels drop below 8 nmol/L.
Common Signs to Watch For
If you suspect your testosterone might be on the decline, see if any of the following sound familiar. These are the most common red flags men report when their levels aren't where they should be.
- Persistent Fatigue: This isn't just feeling tired after a long day. It’s a deep exhaustion that a good night's sleep doesn't seem to fix.
- Reduced Sex Drive (Libido): A noticeable drop in your interest in sex is a classic sign of low testosterone.
- Difficulty with Erections: While many factors can play a part, struggling to get or maintain an erection can be linked to hormonal changes.
- Loss of Muscle Mass: You might find it harder to build or keep muscle, even if you’re still hitting the gym regularly.
Remember, these symptoms can be caused by many different things. Your action is to spot patterns. If several of these resonate with you and persist, it’s a clear signal to investigate further.
On top of these, other clues can include more body fat (especially around your middle), mood swings or irritability, and "brain fog" that makes it hard to concentrate. To dive deeper, explore our comprehensive guide on the signs of low testosterone for a more detailed breakdown.
Lifestyle Factors That Impact Your Hormones

While the natural dip in testosterone levels by age is inevitable, your daily habits determine how steep that decline is. Think of your genes and age as the car you’ve been given – your lifestyle is how you drive it. Making proactive choices can turn what feels like a passive slide into active health management.
Interestingly, UK data shows that even where you live can correlate with your hormone levels, highlighting just how powerful your environment and habits are. Men in London, for instance, tend to have some of the highest average testosterone levels at around 17.2 nmol/L, whereas those in the North East average 15.9 nmol/L.
This difference often comes down to controllable factors like diet, sun exposure, stress, and body weight. If you're curious, you can discover more insights into UK testosterone averages. This proves that the things you can control have a massive impact.
Here are the key areas where you can take direct action to support your hormonal health.
The Power of Movement and Muscle
Exercise is one of the best natural ways to boost testosterone production. To get the most impact, focus on specific types of training.
- Resistance Training: Prioritise lifting weights, especially big, compound movements like squats, deadlifts, and bench presses. These exercises activate multiple large muscle groups at once, triggering a powerful hormonal response.
- High-Intensity Interval Training (HIIT): Focus on short, sharp bursts of maximum effort followed by brief recovery periods. An all-out sprint on a bike is more effective than a long, slow jog for giving your hormones a jolt.
Sleep: The Ultimate Hormonal Reset
You can’t out-train poor sleep. Your body produces most of its testosterone while you rest, making quality sleep non-negotiable.
Skimping on sleep is one of the fastest ways to lower your levels. Consistently getting less than seven hours can slash your testosterone by as much as 15% in just one week—like ageing your hormonal system by a decade, almost overnight.
Your action plan: Make 7-9 hours of quality, uninterrupted sleep a non-negotiable priority. This is the foundation for healthy hormone regulation.
Think of sleep as your nightly hormone factory. Cutting it short is like shutting down the assembly line early—production inevitably drops. Your body simply needs that time to repair, recharge, and regulate its essential systems.
Actionable Steps to Support Healthy Testosterone
Knowing how lifestyle affects hormones is one thing; putting that knowledge into practice is what truly matters. You don't need a complete life overhaul. Instead, focus on making smarter, consistent choices across four key areas to manage the natural decline in testosterone levels by age.
This is your game plan. The goal is to build sustainable habits that create a solid foundation for long-term hormonal balance. These pillars are not separate tasks but interconnected parts of one system. When you improve one area, it naturally lifts the others.
Master Your Nutrition
The food on your plate provides the building blocks for hormones. To give your body what it needs, focus on three key nutrients that are directly involved in testosterone production.
Make these a priority in your diet:
- Zinc: This mineral is vital for testosterone synthesis. Get it from lean red meat, shellfish (especially oysters), seeds, and lentils.
- Vitamin D: Often called the "sunshine vitamin," it acts like a hormone in the body. Find it in fatty fish like salmon and mackerel, and get sensible sun exposure.
- Healthy Fats: Cholesterol is the precursor to testosterone. Include healthy sources like avocados, nuts, olive oil, and egg yolks in your diet.
Action: Build your meals around whole foods rich in these nutrients to supply the raw materials your body's hormone factory needs to run smoothly.
Train Smarter, Not Just Harder
Your workouts should send a clear signal to your body: get stronger. This means prioritising intensity and recovery over simply logging hours at the gym.
For the biggest hormonal impact, build your workouts around large, compound lifts. Incorporate exercises like squats, deadlifts, bench presses, and overhead presses to work multiple muscle groups and trigger a greater testosterone response than isolated movements.
Just as important is what you do after the workout. Overtraining is a killer for testosterone because it elevates cortisol, the stress hormone that works directly against it. Schedule rest days and prioritise sleep to allow your body to repair and grow stronger.
Prioritise High-Quality Sleep
Sleep is when your body performs its most important hormonal work. Your brain signals a major release of testosterone during deep sleep, making 7-9 hours a night an absolute must for keeping your hormones in check.
Consistently skimping on sleep will undo your hard work in the gym and kitchen. Just one week of poor sleep can cause a significant drop in your testosterone levels, effectively fast-forwarding the age-related decline.
Your action plan for better sleep: Stick to a consistent sleep schedule, make your bedroom dark and cool, and avoid screens for at least an hour before bed.
Manage Your Stress Levels
Think of chronic stress as testosterone’s arch-enemy. When you're constantly frazzled, your body pumps out the stress hormone cortisol. High cortisol levels can directly inhibit testosterone production, creating a hormonal imbalance.
While you can't eliminate all stress, you can manage your reaction to it. Implement these simple techniques to make a world of difference:
- Mindfulness or Meditation: Practice for 10-15 minutes a day to lower cortisol levels.
- Deep Breathing Exercises: Use a few minutes of slow, deep breaths to calm your nervous system instantly.
- Get Outside: Spend time in nature, even a quick walk in a park, to help reset your stress response.
By focusing on these four pillars, you create a powerful, combined effect that supports your body from every angle.
When It’s Time to Talk to Your Doctor
Making lifestyle adjustments is powerful, but sometimes not enough. Knowing when to seek a professional opinion is a key part of managing your health. If you’re dealing with persistent symptoms that interfere with your daily life, it’s time to schedule a visit with your GP.
This isn’t about alarmism; it’s about being proactive. A doctor can connect the dots between how you’re feeling and what your blood work says, giving you a complete picture of your hormonal health.
Remember, symptoms like constant fatigue or low mood can have many causes. A proper diagnosis is the only way to know for sure what you're dealing with. Delaying that conversation means you could be missing out on an effective treatment that addresses the root cause.
What to Expect During Your Visit
Discussing low testosterone can feel intimidating, but the process is straightforward. Your GP will want to understand your symptoms, so be prepared to talk about when they started and how they affect you. They’ll ask about your energy, mood, sleep, and sex life.
Based on this conversation, they will likely order a blood test.
This typically measures:
- Total Testosterone: The overall amount of the hormone in your blood.
- Free Testosterone: The unbound, usable testosterone available to your body.
- SHBG (Sex Hormone-Binding Globulin): This shows how much of your testosterone is being 'locked up' and made inactive.
- LH (Luteinising Hormone): This helps determine if the issue originates in the testes or with the signals from the brain.
Your next action step is getting a clear diagnosis. It demystifies what’s happening in your body and provides a clear, evidence-based path forward, whether that involves further lifestyle changes, addressing other health conditions, or considering medical treatment.
This clinical process provides the clarity needed to make informed decisions. It's also worth exploring how supplements can play a supportive role; learn more about the top supplements for hormonal imbalance in our detailed guide.
Got Questions? We've Got Answers

To wrap things up, let's go over some of the most common questions that pop up when talking about testosterone levels and age. Getting these basics down can make a real difference in navigating your health with more confidence.
When Is the Best Time to Get a Testosterone Test?
For the most accurate snapshot, get your blood tested early in the morning, ideally between 7 AM and 10 AM. Your testosterone is naturally at its daily peak during these hours.
Testing later in the afternoon can give an artificially low reading, leading to a misleading picture of your true hormonal baseline.
Are At-Home Testosterone Kits Reliable?
At-home kits can be a handy first step for getting a ballpark figure of your total testosterone, but they don't tell the whole story.
A GP can order a much more detailed panel that includes free testosterone and SHBG, giving you deeper insight. Use at-home kits as a screening tool, but always discuss the results with a doctor to determine the next steps.
While convenient, at-home tests are best used to start a conversation, not to draw final conclusions. A professional medical diagnosis will always provide the most complete and accurate assessment of your health.
How Quickly Can Lifestyle Changes Make a Difference?
Results vary, but you can often feel the benefits of lifestyle changes quickly. Improving your sleep and managing stress can have a noticeable impact on your energy and mood in just a couple of weeks.
Bigger changes, such as those from a new diet or consistent exercise, typically take longer to show up in blood work. You could see substantial improvements within three to six months of dedicated effort.
Is It Possible to Have Too Much Testosterone?
Absolutely. While low T gets most of the attention, excessively high testosterone levels can also be a health concern.
It’s less common, but unnaturally high levels—often from misusing anabolic steroids—can lead to acne, mood swings, and an increased risk of heart issues. The goal is always balance, not just hitting the highest number possible.
Ready to support your hormonal balance and vitality the natural way? The journey to feeling your best starts with giving your body the foundational nutrients it needs to thrive. Oji Shilajit gummies are expertly formulated with over 85 trace minerals, fulvic acid, and powerful adaptogens to help you manage stress, boost energy, and maintain your edge. Discover the benefits of Oji Shilajit today.